Americans are accustomed to taking pills. More than 130 million people (that’s 66% of the adult population) take at least one prescription medication.
It’s sobering that such an expensive — and in some cases, ineffective — system has become the status quo, but most Americans have learned not to question it. We’re less likely to raise our eyebrows at a note that says “Apixaban 2.5 mg, twice daily” than one that reads something like this:
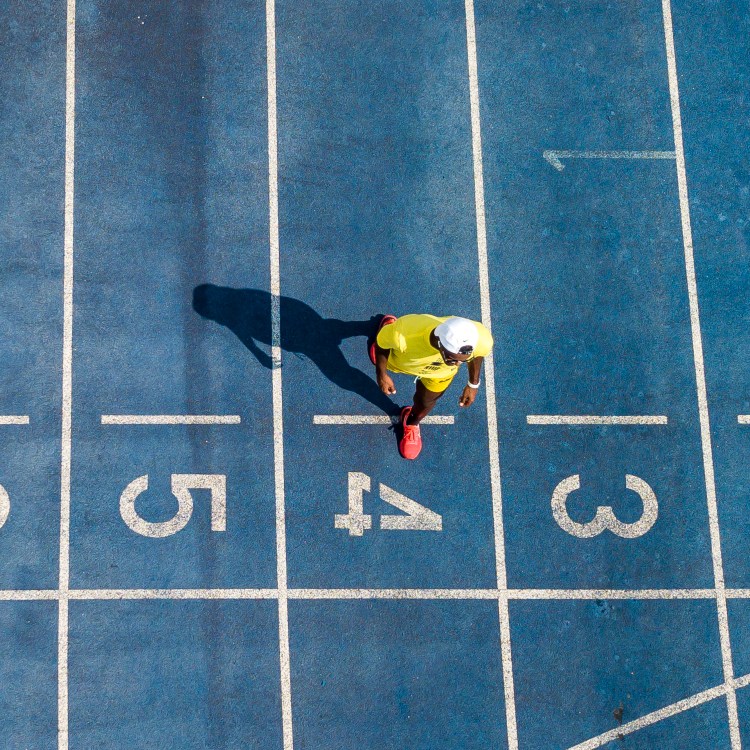
- Moderate aerobic exercise three to four times a week
- Choose from walking, running, hiking, cycling or swimming
- 30 to 60 minutes per session
- Stretch daily, lift weights at least twice a week
And yet, such “exercise prescriptions” have become more popular among physicians in recent years, though, as a complement (or in some cases, outright alternative) to further stuffing their patients’ pill cases. As one doctor shared with The New York Times earlier this year: “[We’re] making, I think, a more holistic assessment of a person’s way of living than maybe we did in the late 1980s.”
It’s one thing for a doctor to tell an adult they see a couple of times a year that they need to drop some pounds and take some pressure off their heart. That probably isn’t breaking news for the patient. But writing those words out in the form of an official prescription lends some professional credence and formality to what otherwise might have been received as passing advice.
By turning an exercise recommendation into a prescription, it A) turns it into a non-negotiable mandate — you know, like taking your medication — and B) offers a repeatable blueprint for those who feel endlessly overwhelmed by the specter of workouts.
While some physicians have started writing exercise prescriptions as an informal way to go above and beyond their normal duties (research indicates that physically active primary care doctors are more likely to prescribe “exercise counseling”) programs have been formalized all around the country; ParkRx, which champions exercise in the outdoors, is a leading example.
Do exercise prescriptions work though? Well, that depends. There’s limited knowledge on whether exercise prescriptions as an institution have been successful; an apathetic patient can just toss the paper in the garbage on the way out of the doctor’s office, and continue living whatever lifestyle they prefer.
When given a chance, though, there’s a mountain of evidence that exercise tacks years onto one’s life. It reduces the burden on the heart, creates new neural pathways in the brain, improves mood and mental health, lowers chronic inflammation, optimizes the immune system…you get it. And an eclectic mix of exercise modes seems to offer the best results, with studies finding benefits from both short-burst HIIT-style sessions and longer, slower Zone 2 training.
Literally any movement is better than none, so from one perspective, doctors can’t go wrong when they jot down a training plan for a willing patient. But exercise prescriptions could soon become more discerning, which will make them even more effective. Consider programs designed to tackle Parkinson’s disease (as discussed in a recent piece by The Washington Post). Some patients have taken control of symptoms that once seemed insurmountable, with an assist from twice-weekly boxing classes.
Ultimately, if you need medication, you need medication. Exercise isn’t trying to supplant science with a more “natural” remedy. But remember: exercise is science, too. And a walk a day, plus a couple strength training sessions each week, just might keep the doctor away.
Thanks for reading InsideHook. Sign up for our daily newsletter and be in the know.